Principles and physical advantages of proton radiotherapy
l Episode 1 What is radiotherapy and what are the advantages of proton radiotherapy?
Radiotherapy, short for “radiation therapy”, is one of the main ways to treat tumors. According to the statistics of international authorities, more than 70% of tumor patients need to receive radiotherapy at different stages of the fight against tumors. Radiotherapy involves irradiating the area where the tumor is concentrated, and the rays pass through the body and directly or indirectly strike the nucleus of the tumor cells. When the DNA double helix inside the nucleus is interrupted by the rays, the tumor cells lose their ability to continue to replicate themselves, or as we say, lose their cloning activity, thus preventing them from continuing to grow. Therefore, radiotherapy is an invisible scalpel.
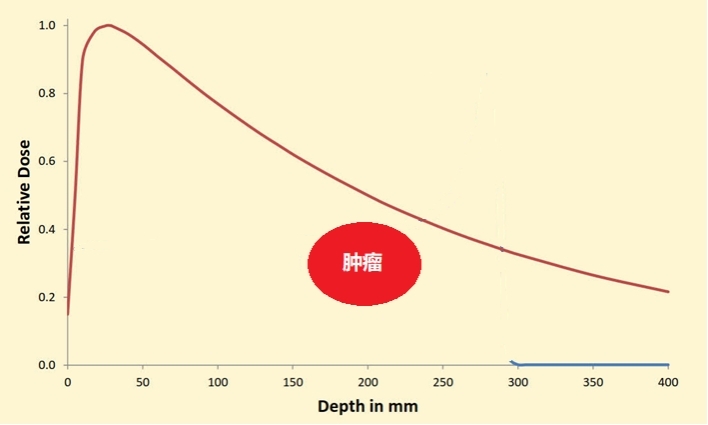
Conventional radiotherapy uses X-rays as a striking weapon. x-rays are photons, which have no weight of their own, so they release their own dose very quickly after reaching the body and continue to fall off with depth. Therefore, on their path to the tumor, the rays are bound to encounter normal cells as well, which are the good guys who are around the battlefield and want to minimize accidental injury. Therefore, protection of the organs surrounding the tumor needs to be achieved by increasing the angle at which the rays enter the body, breaking up the high energy and focusing it on the tumor. However, this approach is like throwing a bomb with a relatively large blast range at the scene of catching bad guys, blowing up the bad guys while inevitably injuring the good guys around the battlefield to a certain extent.
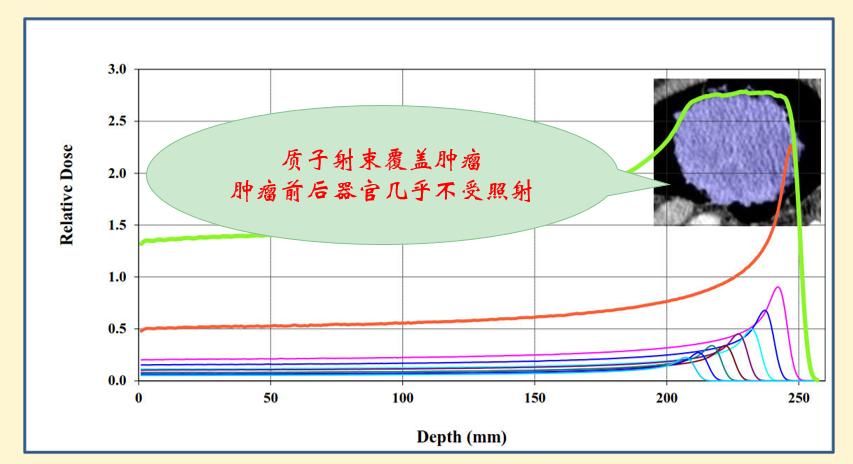
Compared to X-rays, proton rays can strike tumors while better protecting the normal organs around them. This is because a proton is a positively charged and strong muscle man formed by the removal of an electron from a hydrogen atom. When it reaches the body, it releases only a very small portion of the dose and needs to reach a certain depth before it instantly bursts into full energy and then disappears instantly. This creates a peak that we call the Bragg peak.
Therefore, proton radiotherapy is like a drill missile with a more precise blast range, hitting the bad guys while maximizing the protection of the good guys who are around the battlefield. And it is because protons have this characteristic of catching the bad guys and not hurting the good guys that we can make more throws at hitting the bad guys and improve the effectiveness against tumors.
l Episode 2 Which patients are more suitable for proton radiotherapy?
Compared with traditional radiotherapy, proton radiotherapy will better protect the surrounding normal tissues while controlling the tumor. Therefore, as long as patients with solid tumors are suitable for radiotherapy, they can choose proton radiotherapy.
So, which tumor patients will benefit more from it?
Since proton radiotherapy has the characteristics of this kind of drilling missiles and protects the good people around the battlefield, for the following three situations, proton radiotherapy will bring more benefits:
1. the tumor is surrounded by organs that are more sensitive to radiation. For example, if the tumor is in close proximity to vital organs such as the brainstem, spinal cord, and heart, proton radiotherapy can further reduce the extra dose they receive and reduce the risk of complications from radiotherapy.
2. Patients who have undergone radiotherapy but have experienced recurrence. Since the original radiotherapy process has already caused some additional radiation to the surrounding organs, more attention should be paid to protect the function of the surrounding organs when undergoing radiotherapy again.
3. Children with tumors. Statistics show that the fatal risk of tumor to children ranks second only to accidental injuries, but the good news is that the cure rate of pediatric tumor patients is much higher than that of adult tumor patients, and most of the children can grow up to adulthood after timely and standardized treatment. Therefore, it requires us to pay more attention to the side effects that may be brought to children during tumor treatment. Therefore, it is very important to implement proton radiotherapy for pediatric tumor patients to maximally protect the function of the surrounding organs and give the children who have overcome the tumor a healthy growth process.
l Episode 3 What is the general process of proton radiotherapy?
The general process of proton radiotherapy is not significantly different from conventional X-ray radiotherapy. Radiotherapy tumors have to be struck with a steady and accurate blow, and additional radiation to the surrounding organs has to be avoided as much as possible, so the precision of our rays striking the tumor has to be sub-millimeter, sub-millimeter precision. In proton radiotherapy, we have to accurately superimpose the Bragg plateau on the tumor location, and a slight deviation will make part of the bad guys miss the net, i.e., the tumor does not get effective irradiation, and make part of the onlookers suffer, i.e., cause mis-irradiation of the surrounding organs. Therefore, proton radiotherapy requires higher precision. We propose that radiotherapy should achieve “three precision”.
The first is precise positioning. Positioning is to conduct CT or MRI scanning with the patient in a fixed position. With the help of vacuum pads, thermoplastic film, position frames and other devices, the patient's position is fixed on the CT or MRI scanning bed, and patient-specific positioning instruments are made. The patient's image obtained from the scan fully demonstrates the anatomical relationship between the tumor and the surrounding normal tissues and sensitive organs in the body, which is like a topographical map of the battle of radiotherapy, showing the enemy and the good guys and their positions at a glance. This process is the first part of radiotherapy and lasts about 20-30 minutes.
The second step is precise planning. The battle terrain map obtained from the positioning is sent to the command, which is the radiotherapy planning system. Together, the radiotherapists and physicists develop a battle plan to combat the tumor. They plan from which angles, in what shape and with what intensity the rays will hit the patient, and then simulate the effect of the blow, i.e. the distribution of the radiation dose in the body, by computer. It is assessed that the tumor has been sufficiently and adequately struck without serious effects on the surrounding organs, and this is then ready to be submitted to the operational department for a strike. This process is critical and requires the involvement of clinicians and physicists and is usually completed 2-3 days after the first step of localization.
The third step is to administer the blow. Radiotherapy is overwhelmingly delivered in multiple sessions, as few as 3 or 5 or as many as 20 or 30, depending on the condition and the radiotherapy technique used. Typically, radiotherapy is administered once a day, five days a week. The procedure for each radiotherapy session is as follows: the radiotherapy technician guides the patient into the treatment room and, with the help of the patient's exclusive positioning device, restores the patient's position on the treatment bed. In order to ensure that the rays have a good effect on the
